Are you puzzled by irregularities in your menstrual cycle? Or maybe you’re not sure what exactly constitutes an abnormal period? Media depicts periods as being painful, moody, and so taxing that they lay us out completely – so it’s common that we think that this is what periods are meant to be like.
Let’s do a quick calculation so we can let the implications of that settle in..
The average person gets their period around 12 years old, and the average age of menopause is 51. That’s 39 years of painful periods. With the average cycle length of 5 days per month, with 12 months in the year.. that equals a whopping 2,340 days of suffering. That’s 6 years of suffering!
This is something we take very seriously. The good news is, there are many ways to address it beyond the often-prescribed birth control pill (which, contrary to popular belief, isn’t a cure-all!). In fact, various lifestyle changes can make a significant difference.
Let’s break down what constitutes an abnormal period, how to recognize the signs, and the factors that can influence your menstrual health. Here’s a detailed exploration to help you gain clarity on abnormal periods and take control of your reproductive well-being.
What is an abnormal period?
1. Changes in Cycle Length: Irregular cycle lengths, such as cycles shorter than 21 days or longer than 35 days
2. Unpredictable Bleeding: Unusual or unpredictable bleeding patterns, including spotting between periods or heavy bleeding, may signify irregularities.
3. Missed Periods: Prolonged absence of menstrual periods (amenorrhea) or skipped cycles without pregnancy can be indicative of irregular menstruation.
4. Unusual Flow: Abnormally light or heavy menstrual flow compared to your typical pattern may suggest irregular periods
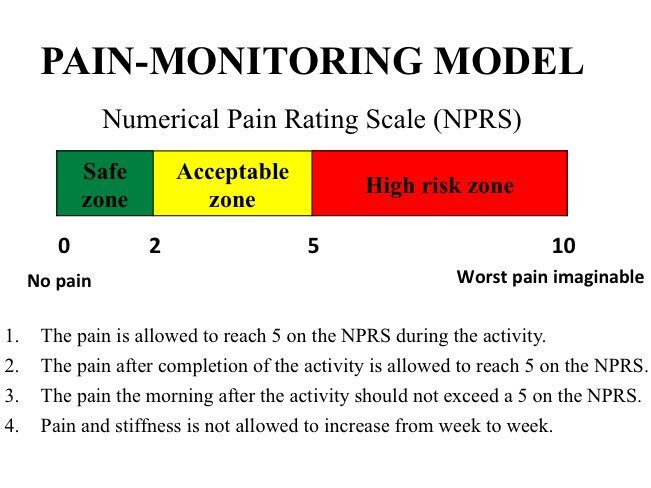
5. Severe Pain: Experiencing intense menstrual cramps (dysmenorrhea) or pelvic pain beyond normal discomfort levels could be a sign of abnormal periods.
6. Heavy period: bleeding more than 80 mL (which is the equivalent of 8-9 fully soaked regular tampons–for the whole cycle, yes it is alot less than we normalize, but note that you may use more tampons than this that aren’t fully soaked).
7. Painful period: if you are having more than slight cramping on your first day, this is considered abnormal
8. Constipation: unable to poop, or having irregular poops (or straining or pain with pooping)

Identifying Abnormal Periods:
Keeping a menstrual diary or using a period tracking app can assist in monitoring your cycle and identifying any irregular patterns. Look out for recurring symptoms such as unusually heavy or light bleeding, severe cramps, prolonged periods, or erratic cycle lengths as potential indicators of abnormal menstruation. This is crucial to know what is normal or not for yourself.

Role of Cortisol & Estrogen Dominance:
Cortisol, the stress hormone produced by the adrenal glands, can impact menstrual regularity by influencing hormone levels and disrupting the bodies ability to make progesterone, leading to estrogen dominance. When the body is stressed, instead of making enough progesterone, it makes cortisol. Elevated cortisol levels can lead to an impaired progesterone to estrogen ratio due to chronic stress. This can interfere with ovulation and menstrual cycle regulation, contributing to irregular periods.
Pelvic Heaviness and Low Back Pain:
Pelvic heaviness, often associated with conditions like uterine fibroids, endometriosis, or pelvic organ prolapse, can lead to discomfort in the lower back. The strain on the uterosacral ligament from pelvic heaviness can radiate to the lower back, causing pain and stiffness in the lumbar region.
Understanding Insulin Resistance:
Insulin resistance, a metabolic condition characterized by decreased sensitivity to insulin, can disrupt hormonal balance and impact menstrual health. Elevated insulin levels can trigger an excess (or reduction) of androgen production (ie testosterone), disrupting ovulation and leading to irregular periods, lack of ovulation, or fertility issues.

Vitamins:
One study showed that that many people who have painful periods may be low in zinc, B 12 and vitamin D
Impact on Menstrual Cycle:
Insulin resistance-induced hormonal imbalances can manifest as irregular periods, cycle disturbances, or fertility challenges. The dysregulation of ovarian function and hormone levels can affect ovulation, leading to menstrual irregularities and cycle disruptions.
Common culprits:
Oftentimes painful or irregular periods can be caused by polycystic ovarian syndrome (PCOS), endometriosis, perimenopausal changes, all of which the information here can help with.
3 Practical Tips for Menstrual Health:
1. Realistic Stress Management:
While it can be challenging in a world filled with stress, try to take a moment to observe your daily interactions. Reflect on your relationships—whether at work, with friends, or in romantic settings—and notice situations or environments where you may feel constrained or judged.
Although identifying stress triggers can be challenging initially, the first step is to simply pay attention to how your body responds in various settings. The more aware you become, the easier it is to make changes that lower your cortisol and daily stress levels. Setting boundaries and being mindful of the people you spend time with can significantly help. Over time, this approach allows you to experience greater joy in your life and naturally reduces the body’s stress response, offering a more sustainable way to manage stress.
Other suggestions include:
- Limiting social media usage (especially before bed and first thing in the morning)
- Walking in nature
- Breathwork: inhaling for 4 seconds, holding for 4 seconds and exhaling for 4 seconds for a couple minutes throughout the day can help to reduce stress and anxiety
- Reduce preventable stressors ahead of time, so that your body is able to react with more resilience during unpredictable times.
- For example, leaving earlier (what you can control) for an appointment in case there is traffic (unpredictable)
- Pay attention to your inner dialogue—do you often criticize or judge yourself? Try to show yourself some compassion; remember, you’re human, doing your best in a challenging world.

2. Intentional Nutrition:
Choose a diet rich in nutrients, including whole foods, fiber, and protein, to enhance insulin sensitivity and support hormonal health. Adding a protein to a carbohydrate is a great way to start stabilizing your blood sugar (e.g. having an egg with toast). It’s important to have a balance and remember that occasional enjoyment of your favorite foods are part of a healthy living.
Consistency in your everyday dietary choices is important, but be kind to yourself and try to avoid shaming yourself for occasional deviations from your routine. Life is full of special occasions like birthdays, travel, and celebrations, and it’s essential to enjoy these moments without guilt. Rather than using dietary guidelines as a means of self-judgment, view them as a helpful framework to guide your choices and nourish your body without unnecessary pressure or negativity.

3. Regular Exercise:
Strength training plays a pivotal role in the body’s glucose metabolism as muscles require glucose for optimal function. By engaging in strength training exercises, the muscles utilize glucose effectively, leading to lower sugar levels in the bloodstream and subsequently reducing symptoms of insulin resistance. Additionally, walking serves as a beneficial activity for stabilizing blood sugar levels. As the body utilizes glucose for energy during walking, it helps maintain stable blood sugar without exerting excessive strain on the body. Incorporating both strength training and walking into your routine can support glucose regulation and overall metabolic health.
By understanding the nuances of abnormal periods, addressing cortisol levels, pelvic heaviness, insulin resistance, and implementing lifestyle adjustments, you can empower yourself to optimize menstrual health and overall well-being.
Don’t settle for losing six years of your life to pain just because society has normalized it—we won’t accept that!.
References:
Guntupalli, S. K., & Setji, T. L. (2023). The impact of insulin resistance on hormonal regulation and reproductive health. Journal of Clinical Endocrinology, 12(3), Article 10244367.
Naraoka, Y., Hosokawa, M., Minato-Inokawa, S, & Sato, Y. (2023). The effects of lifestyle factors on menstrual pain severity: A population-based study. Journal of Women’s Health Research, 11(2), Article 10178419.
Elara Care. (n.d.). How cortisol affects women’s health and the menstrual cycle. Elara Care. Retrieved from https://elara.care/hormones/how-cortisol-affects-womens-health-and-the-menstrual-cycle/