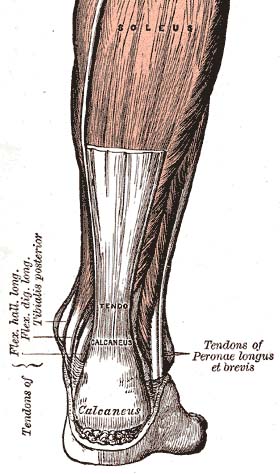
Achilles tendinitis refers to painful overuse injury of the tendon that connects your heel to your calf muscles. It impacts numerous people – from athletes in running and jumping sports, to individuals who lead less active lifestyles. The pain and stiffness can greatly impact basic quality of life including activities like walking, exercise, and going up and down stairs.
Before we dive into common treatments for this issue, it’s worth discussing exactly what it is, right down to how clinicians define and classify it. Having a better understanding of the diagnosis makes for more effective treatment approaches. We’ll start with the changing terminology – it turns out that “tendinitis” doesn’t quite capture what’s happening since the underlying issue is not quite black & white. Without further adieu, let’s break down the evolving terminology and science-backed treatment approaches:
What’s Up with the Changing Terminology?
Let’s first describe the key differences between tendinitis, tendinosis and tendinopathy, because these terms are NOT interchangeable.
- Tendinitis has historically been used to describe inflammation of a tendon, with treatments focused on reducing that inflammation.
- Tendinosis refers to more degenerative changes and microtears of the tendon, without inflammation present.
- Tendinopathy is the most broad term that encompasses all tendon disorders, including inflammatory and degenerative features. It can involve inflammatory elements right after injury, but typically it’s more to do with dysfunctional healing and tissue remodeling over time.
What we have a better understanding of now is that there is a spectrum of issues that can impact tendons, many of which are improper remodeling or healing of the tissue, as opposed to simply inflammation. Treatments (as discussed later) should focus more on remodeling and regeneration of the tendon rather than simply reducing inflammation. We need to get that tissue strong and resilient again!

What Causes Achilles Tendon Issues?
Simply put, it’s an overuse injury from repetitive strain. Micro-tears in the tendon outpace the tendon’s ability to repair itself properly, thus resulting in pain and dysfunction. Things like calf tightness, overpronation, sudden jumps in activity (i.e. couch to 5k), and poor leg strength may contribute over time.
Most patients do not experience a single event or injury, but rather smaller insults over time. Pain can set in over days to weeks, and may worsen depending upon the person’s activity. So oftentimes a cycle of rest or stopping activity completely followed by resuming activities without the proper interventions in between causes people to stay in this unfortunate pain cycle. Complete rest actually increases tendon dysfunction!
Pain usually goes through a “warm-up phenomenon.” This means that pain can improve with exercise/activity a bit, only to return with a vengeance later on or the next day. This is where a structured program and guidance from an expert clinician is crucial.

How Does Physical Therapy Get You Back on Track?
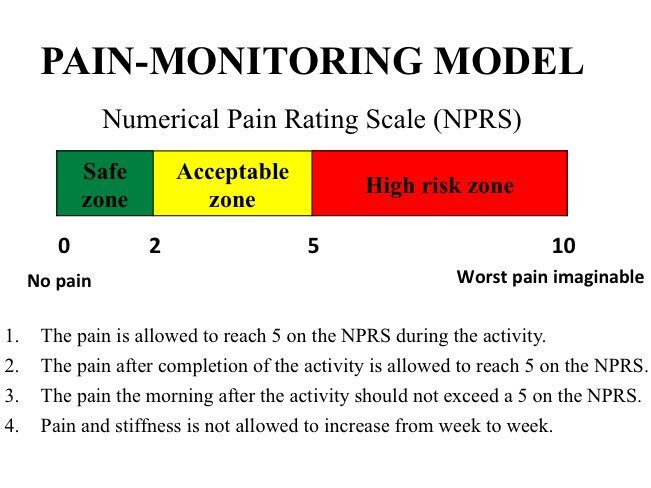
Your physical therapist should develop a customized treatment plan aligned with current evidence-based clinical guidelines and your goals (We do at ResilientRx)! Properly dosed strength exercises, mobility training, biomechanical corrections, and guidance on gradual return to activity aim to spark tissue regeneration/remodeling while minimizing flare-ups. Guiding the optimal balance of rest and activity helps manage load demands. It’s an intricate puzzle tailored to each patient. It’s also important to note that rehab will not be PAIN-FREE. It’s actually safe to have mild levels of tendon pain lasting less than 24 hours after activity. We often use a simple scale to monitor pain levels, which helps to dose exercise appropriately and push things forward without compromising progress. Every patient will respond differently, so communication is key.
Here’s what the framework for achilles tendinopathy rehab looks like:
- Early stage: hands-on modalities to calm symptoms such as soft tissue work/massage, joint mobilizations, dry needling and taping. Here we also introduce gentle strength and mobility exercises to start the tissue remodeling process
- Mid stage: progressive loading via strength exercises to the gastroc and soleus (calf muscles). Isometric and eccentric exercises are advanced to further expose the tendon to more time under tension Stretching may be more tolerated in this phase compared to when symptoms are more acute.
- Late stage: we start to move more toward plyometrics exercise and sport-specific or functional training as needed, including more “traditional” strength training principles
The Bottom Line
Tendinopathy rehab is load-related and dose-dependent. We want the achilles tendon to tolerate higher loads over time, so this is a gradual process that requires patience and diligence. The unfortunate truth however, is that progress with Achilles tendinopathy is almost never linear. There will be ups, downs, and plateaus. Sometimes consistent strength training may need to be done for anywhere from 3-6 months before returning to plyometrics. Anti-inflammatories and complete rest are discouraged as this leads to further deconditioning, weakness, and more susceptibility to flare-ups. The good news is that over 75% of tendinopathy patients achieve resolution of symptoms through dedicated rehab and avoid surgery! It can be a long road for many of us, but we’re here for you!
Have you been struggling with Achilles tendinitis or chronic tendon pain in general? Schedule an appointment with one of our Doctors of Physical Therapy to get you back to doing the things you love! CLICK HERE or call 512-777-0330.
References:
1. Magnan B, Bondi M, Pierantoni S, Samaila E. The pathogenesis of Achilles tendinopathy: a systematic review. Foot Ankle Surg. 2014;20(3):154-159. doi:10.1016/j.fas.2014.03.002
2. Morrissey D, Roskilly A, Twycross-Lewis R, et al. The treatment of mid-portion Achilles tendinopathy: a systematic review. J Foot Ankle Res. 2021;14(1):3. Published 2021 Jan 11. doi:10.1186/s13047-020-00440-5
3. van der Plas A, de Jonge S, de Vos RJ, et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med. 2012;46(3):214-218. doi:10.1136/bjsm.2010.083428
4. Rowe V, Hemmings S, Barton C, et al. Conservative management of midportion Achilles tendinopathy: a mixed methods study, integrating systematic review and clinical reasoning. Sports Med. 2012;42(11):941-967. doi:10.1007/BF03262301
5. Doral MN, Alam M, Bozkurt M, et al. Functional anatomy of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):638-643. doi:10.1007/s00167-010-1083-7
6. Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med. 2003;22(4):727-741. doi:10.1016/s0278-5919(03)00034-7
7. Padhiar N, Achana F, Davies A, et al. Eccentric exercises reduce the risk of Achilles tendon overuse injury: a systematic review and meta-analysis. Br J Sports Med. 2021;55(21):1180-1188. doi:10.1136/bjsports-2020-103426




