Physical Therapy for Menopause Wellness
Let us guide you through menopause with knowledge and empowerment, free from judgment or gaslighting

Physical Therapy for Menopause Wellness

Let us guide you through menopause with knowledge and empowerment, free from judgment or gaslighting
Are you experiencing the early stages of peri-menopause and feeling out of touch with your body? If you’re between 40-50 years old and noticing significant changes in your body, you may be unsure if you’re entering peri-menopause. Physical therapy for menopause can help. You can also learn more about other pelvic floor therapy treatment options here.
Peri-menopause is the transitional phase before menopause, lasting an average of 4-8 years. During this time, estrogen and progesterone levels begin to decline. Decreased progesterone levels can lead to joint pain and muscle soreness, while reduced estrogen levels may cause symptoms like muscle weakness, vaginal dryness, and incontinence.
Menopause is officially reached after 12 consecutive months without a menstrual cycle, marking the post-menopausal stage. On average, menopause occurs around age 51, but the timing varies among individuals. It can occur earlier or later, especially if menopause is induced by medical reasons such as a radical hysterectomy or cancer treatments.
Navigating these changes can feel overwhelming, especially as you approach mid-life. Balancing responsibilities like caring for aging parents, becoming an empty nester, and managing career or relationship changes can leave you feeling like you’ve neglected self-care.
The physical and emotional transformations during peri-menopause and menopause can be challenging, especially without a supportive healthcare team to guide you through. You may feel overlooked or misunderstood by healthcare providers, adding to your anxiety.
We are here to offer support and acknowledge the validity of your symptoms. You can learn more about physical therapy and additional resources that can help on our podcast here.
Peri-menopausal people
reported that their healthcare team did not take their symptoms seriously
Post-menopausal people
experience vaginal changes
Peri-menopausal people
experience increased muscle & joint pain


What is Physical Therapy for Menopause?
Our team specializes in physical therapy for menopause and perimenopause changes. We help you understand the changes in your body and empowering you to prioritize your well-being.
Common symptoms we address include constipation, generalized weakness, increased urge to urinate, urinary and/or fecal leakage, pain during sex, recurring UTIs, chronic pain flare-ups, pelvic organ prolapse, and nervous system regulation.
We provide assistance in reducing the risk of osteoporosis through safe strength training education, making the gym less intimidating for those new to weightlifting during this phase of life.
Our focus is on educating you on the mind-body connection, empowering you to take control of your health journey. Stress can exacerbate symptoms during this period, so understanding this connection can have a transformative impact on your well-being.
Consider this an investment in your overall health, enabling you to advocate for your healthcare needs and trust your body, whether you choose hormone therapy or not.
Age-related judgment, gaslighting, and lack of support from the healthcare system can be overwhelming for individuals in this phase of life. We are here to provide assistance and support.
Diagnoses That We Treat…

Re-occuring Urinary Tract Infections
What Is It?
An increase in urinary tract infections is common during this time. This is often due to the change in vaginal pH resulting from lower vaginal estrogen levels.
This change can irritate the tissue around the urethra, making it more prone to infection.
Understanding vaginal health, bladder health, and restoring vaginal pH (even without estrogen) can be very beneficial during this period.
Many people complain that they:
- Needing to take antibiotics frequently
- Concerns about penetrative sex due to UTI occurrence
- Increased urge to urinate
- Vaginal dryness
Urinary Incontinence
What Is It?
This is accidental leakage or increased urgency to urinate often. Many people believe they simply need to accept it because they were pregnant or aging- this is not true!
This can be successfully treated in pelvic floor physical therapy.
Many people complain that they:
- Pee with they sneeze or cough
- Fear they will leak when running or jumping
- Fear not being around a restroom because of an urgency to pee often

Urinary Incontinence
Prolapse
Prolapse
What Is It?
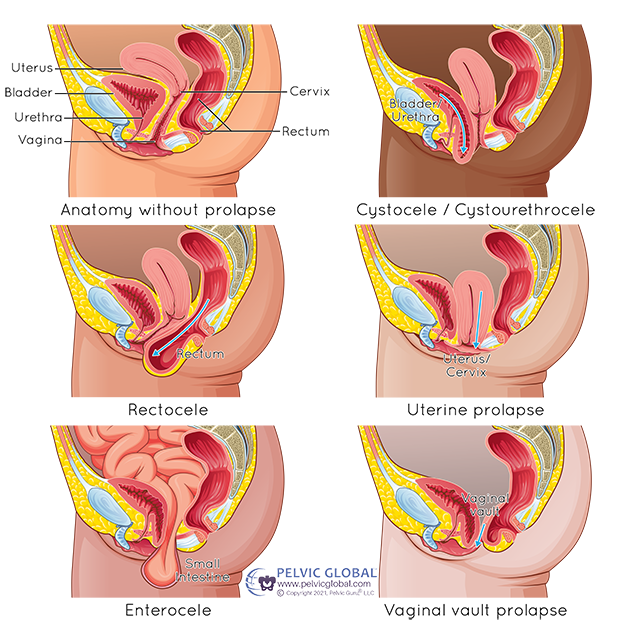
This is when the pelvic organs start to “fall down” into the vagina. The image shows the different types of pelvic organ prolapse.
Many people complain that they:
- Feel heaviness in the bladder, back or around the vaginal opening or anus
- Feel like they are wearing a tampon
- Notice bulging around the vagina or anus
- Experience double voiding, aka peeing a few minutes after you already have
Pain with Sex
What Is It?
Pain with sex is unfortunately a common dysfunction of the pelvic floor associated with menopause. This can be due to the change in the vaginal pH, pelvic floor tension, and/or impaired hip/pelvic mobility. However, there are a variety of treatments that can help.
Many people complain that they:
- Cannot tolerate any vaginal penetration
- Have pain with deep penetration and initial penetration
- Have pain or discomfort in certain sexual positions
- Vaginal dryness or burning
- They cannot feel as much sensation as they did prior, and mainly feel pain

Pain with Sex

Constipation
What Is It?
Constipation generally means there is a difficulty in having a bowel movement, which can also include straining, harden feces and/or having less than 3 bowel movements a week.
This is often a symptom during peri-menoapuse as estrogen and progesterone decrease. This can slow down digestion and cause a decrease in pelvic floor coordination.
Many people complain that they have:
- More pain with pooping
- Pelvic/abdominal/back pain
- Increased bladder symptoms when constipated
- Increase of hemorrhoids or anal pain.
- Painful bowel movements
- Heaviness in the pelvis
Osteopenia and Osteoporosis
What is it?
As estrogen decreases, this increases risk of developing osteoporosis which is weakening of the bone causing increase risk for fractures.
Increasing muscle strength through weight training has been shown to improve bone density.
Many people complain that:
- They want to weight train but are unsure how to do it
- Feel most gyms or classes focus on people in their 20s-30s
- Intimidated by gym environments
- Worried about injuring themselves when lifting weights and need direction


Increased Muscle and Joint Pain
Increased Joint Pain, Muscle Pain and Headaches
What Is It?
As peri-menopause progresses, the decrease in estrogen causes muscle weakness while the decrease in progesterone can increase joint pain and stiffness
Many people complain that:
- Feel dismissed by other health care practitioners who say your symptoms “due to age”?
- Are feeling more pain than normal
- Increased migraine or headache frequency or intensity
- Increased anxiety and muscle tension
Medically Induced Menopause
What is it?
This is when menopause is medically induced earlier than expected due to a radical hysterectomy, and/or cancer treatments that include: radiation and/or chemotherapy.
Most commonly this can be due to treatments for breast, ovarian, vaginal, cervical or uterine cancers.
Many people complain about:
- Heaviness in the pelvis
- Pelvic pain
- Pain with sex
- Vaginal dryness/pain
- Accidental leakage (bowel or bladder)
- Muscle tightness post radiation

Medically Inducted Menopause due to Cancer Treatments
FAQ
I am on my period, can I still come for an appointment?
Yes! We can complete all activities externally if you are not feeling well enough for an internal assessment.
How many visits will I need?
Each diagnosis is different. It depends on the diagnosis, how long it has been occuring for and symptom intensity. We will make recommendations on how often to attend after your initial evaluation, but we work with your budget and time to make the best possible plan to fit your needs.
Because we are 1:1 you the full time, most people only need to come anywhere from 6-10+ visits, usually once a week.
What is an internal assessment?
An internal assessment is when your physical therapist assesses the 3 layers of the pelvic floor through the vagina or rectum. We also assess strength and coordination as well. However, if you are uncomfortable with this, we can complete everything externally.

