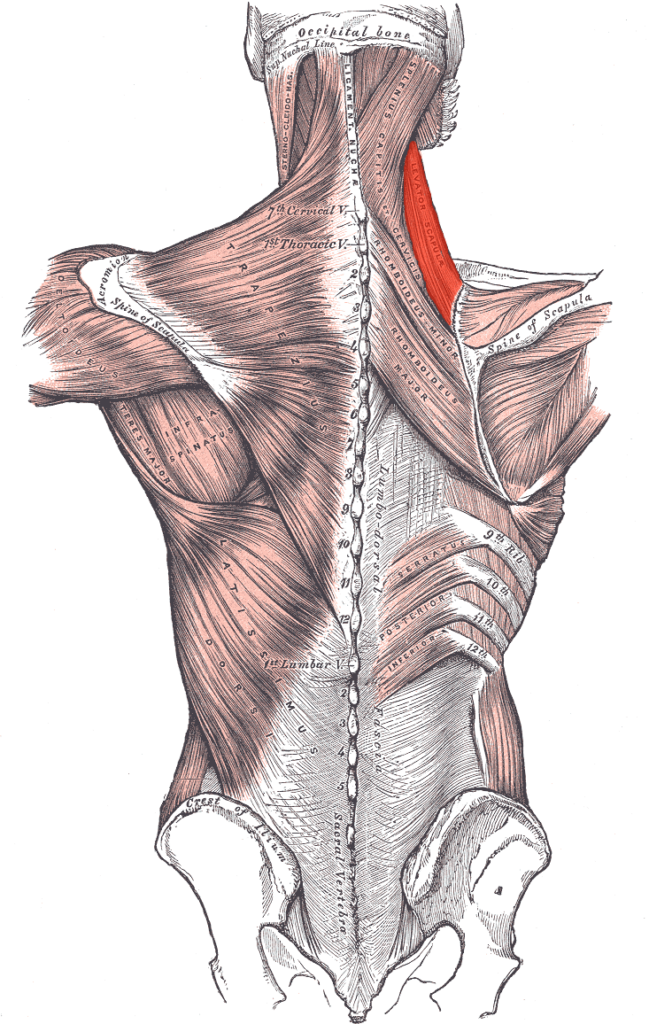
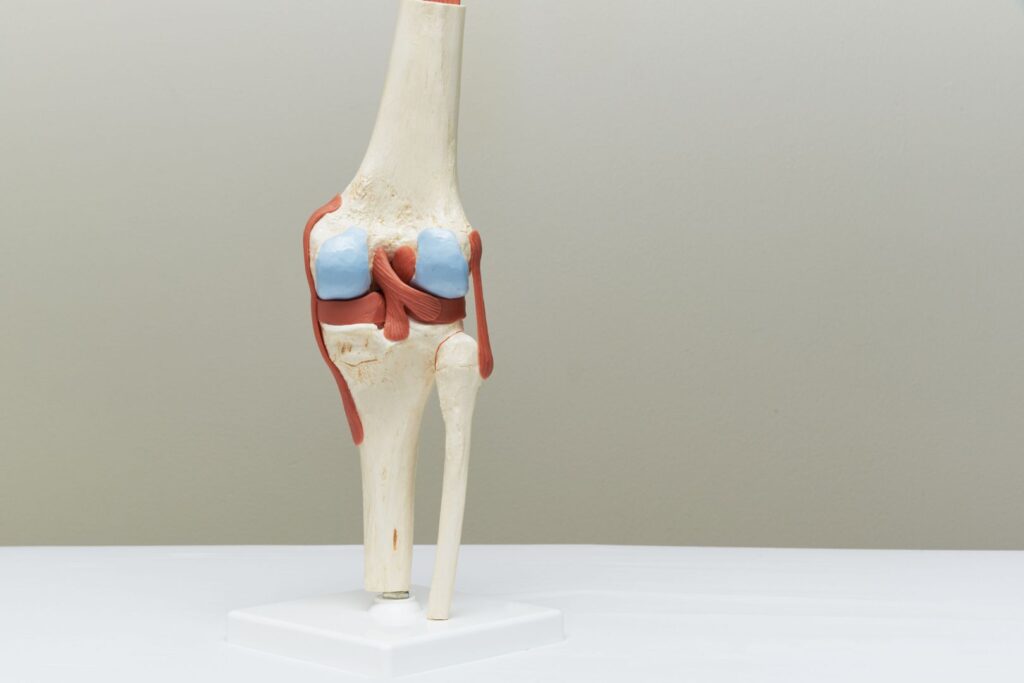
When it comes to knee injuries, meniscus tears are a very common diagnosis and occur across multiple age groups. It’s estimated that the annual incidence of meniscus tears ranges from 60 to 70 cases per 100,000 people. The menisci are two C-shaped pieces of cartilage that play a vital role in cushioning and stabilizing the knee joint. Meniscus tears can occur generally in 2 ways: due to acute trauma or due to degeneration. Acute injuries involve twisting or impact while degenerative tears can occur due to factors such as lifestyle, general health (comorbidities), prior injuries, and genetics. Approximately 35% to 50% of individuals over the age of 65 have meniscus tears. In contrast, traumatic meniscus tears from sports or other physical activities are more frequently seen in adolescents and young adults. For both traumatic or degenerative tears, individuals can experience pain, swelling, limited mobility and impaired function.
It may seem that surgery is the only answer to fix these issues, however emerging research suggests that conservative management is a very viable alternative to surgery in MANY cases. In this blog, we will delve into the topic of meniscus tears and explore the growing body of evidence that supports conservative management over arthroscopic surgery. In fact, outcomes tend to be the same, if not better, when people rehab their knee instead of jumping right to the operating table.
Conservative Management: The Evidence
A robust body of research exists that shows the effectiveness of conservative management is just as good, if not better, than arthroscopic knee surgery, which includes physical therapy (exercise), activity modification, and pain management. Briefly summarized below are some key research findings in support of a conservative approach:
The FIDELITY Trial:
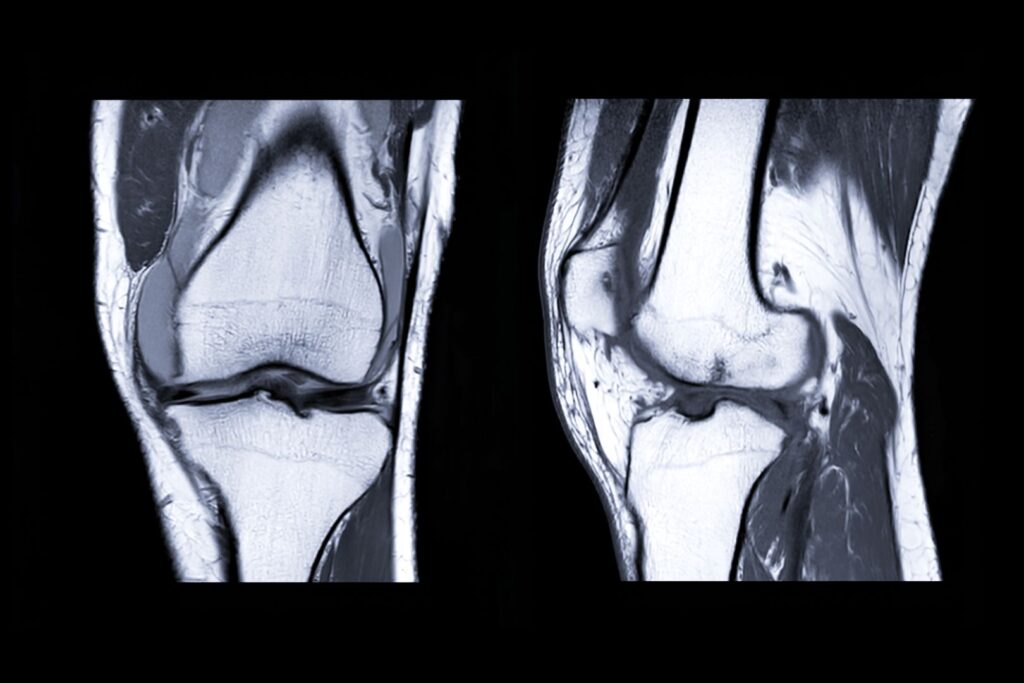
FIDELITY (Finnish Degenerative Meniscal Lesion Study) trial evaluated the outcomes of arthroscopic surgery versus sham surgery (placebo) for degenerative meniscal tears. The results revealed that there were no significant differences in pain or functional improvement between the two groups at 12-month follow-ups.
ESCAPE Trial:
The ESCAPE research group looked at nonobstructive degenerative meniscus tears in patients over the age of 45, and compared arthroscopic partial meniscectomies to physical therapy. They found no significant or clinically relevant difference in knee function at 5-year follow up between the two groups. The findings of this trial support the recommendation that exercise-based physical therapy should be the preferred treatment over surgery for degenerative meniscal tears.
The METEOR Trial:
The Meniscal Tear in Osteoarthritis Research (METEOR) trial focused on patients with meniscal tears and knee osteoarthritis. The study compared the outcomes of arthroscopic surgery with those of physical therapy alone. Surprisingly (or not surprisingly), the results showed that physical therapy alone was as effective as surgery in improving pain and function at 6-month and 12-month follow-ups.
The Benefits of Nonsurgical Treatment

Conservative management offers several advantages over surgery for meniscus tears, including:
Avoiding unnecessary risks: Arthroscopic surgery carries inherent risks such as infection, blood clots, and anesthesia complications. Opting for conservative management reduces exposure to these risks.
Cost-effectiveness: Surgery can be costly, especially when factoring in pre-operative assessments, post-operative care, and rehabilitation. Conservative management offers a more cost-effective alternative.
Preserving meniscal tissue: The menisci play a crucial role in knee function and joint stability. By avoiding surgery, there is a higher chance of preserving the meniscal tissue, reducing the risk of long-term complications such as osteoarthritis. In fact, patients who undergo meniscectomies increase their likelihood of needing total knee replacement down the road.
Faster recovery: Surgery typically requires a more extended recovery period, involving restricted movement and rehabilitation. Conservative management allows patients to engage in tailored physical therapy programs that can promote faster recovery and return to normal activities.
Summary
Surgeries (even simple, less invasive ones like knee arthroscopies) always come with potential risks and complications, and could lead to accelerated progression of knee osteoarthritis later in life. Individuals with significant, obstructive meniscus tears (i.e. knee locking) may still require surgical intervention. However the research is very convincing that most meniscus tears, especially degenerative, are better treated with a nonsurgical approach and that arthroscopic surgery is not superior to physical therapy intervention.
Have you been diagnosed with a meniscus tear or have ongoing knee pain? Schedule an appointment with one of our Doctors of Physical Therapy to get you back to doing the things you love! CLICK HERE or call 512-777-0330.

References:
Hede, A., Jens|n, D. B., Blyme, P., & Sonne-Holm, S. (1990). Epidemiology of meniscal lesions in the knee: 1,215 open operations in Copenhagen 1982-84.Acta orthopaedica Scandinavica. 1990; 61(5): 435-437.
Goyal, D., Keyhani, S., & Lee, E. H. (2012). HHS public access. Annals of Internal Medicine, 156(12), 945–957. doi: 10.1059/0003-4819-156-12-201206190-00006
Paxton, E. S., Stock, M. V., Brophy, R. H., & Lubowitz, J. H. (2013). Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy – Journal of Arthroscopic and Related Surgery, 29(3), 872–880. doi: 10.1016/j.arthro.2012.12.022
Englund, M., Guermazi, A., Roemer, F. W., Aliabadi, P., Yang, M., Lewis, C. E., … Nevitt, M. C. (2008). Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis and Rheumatism, 58(3), 810–816. doi: 10.1002/art.23293
Sihvonen, R., Paavola, M., Malmivaara, A., Itälä, A., Joukainen, A., Nurmi, H., … & Järvinen, T. L. (2018). Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Annals of the rheumatic diseases, 77(2), 188-195.
Hwang, Y. G., & Kwoh, C. K. (2014). The METEOR trial: no rush to repair a torn meniscus. Cleveland Clinic Journal of Medicine, 81(4), 226-232.
Noorduyn, J. C., Van De Graaf, V. A., Willigenburg, N. W., Scholten-Peeters, G. G., Kret, E. J., Van Dijk, R. A., … & ESCAPE Research Group. (2022). Effect of physical therapy vs arthroscopic partial meniscectomy in people with degenerative meniscal tears: five-year follow-up of the ESCAPE randomized clinical trial. JAMA Network Open, 5(7), e2220394-e2220394.