SIJ & Hip Specialists in Austin TX
Get to the root of your pain from a pelvic floor and whole body perspective. We treat the cause, not just the symptoms, for lasting relief and real results

SIJ & Hip Specialists in Austin, TX

Get to the root of your pain from a pelvic floor and whole body perspective. We treat the cause, not just the symptoms, for lasting relief and real results. Work with our hip specialists to learn more!
Lower back, hip, and SI joint pain shouldn’t be your new normal. ResilientRx helps you move better, without band-aid fixes.
Many of our clients come to us after seeing multiple providers often without lasting relief.
Not because they weren’t trying, but because their symptoms weren’t being addressed from a whole-person perspective.
Fascia, lymph, the pelvic floor, thoracic mobility, gait, hormone changes, such as peri-menopause, and the nervous system all play a role in how we move and feel. Ignoring any of these layers means missing the root cause.
At ResilientRx, we blend a modern, evidence-based approach with mind-body-soul integration. We teach you how your body actually works, so you can take that knowledge with you, long after the sessions end. All of our physical therapists are hip specialists to ensure quality results.
Hip Labral Tear
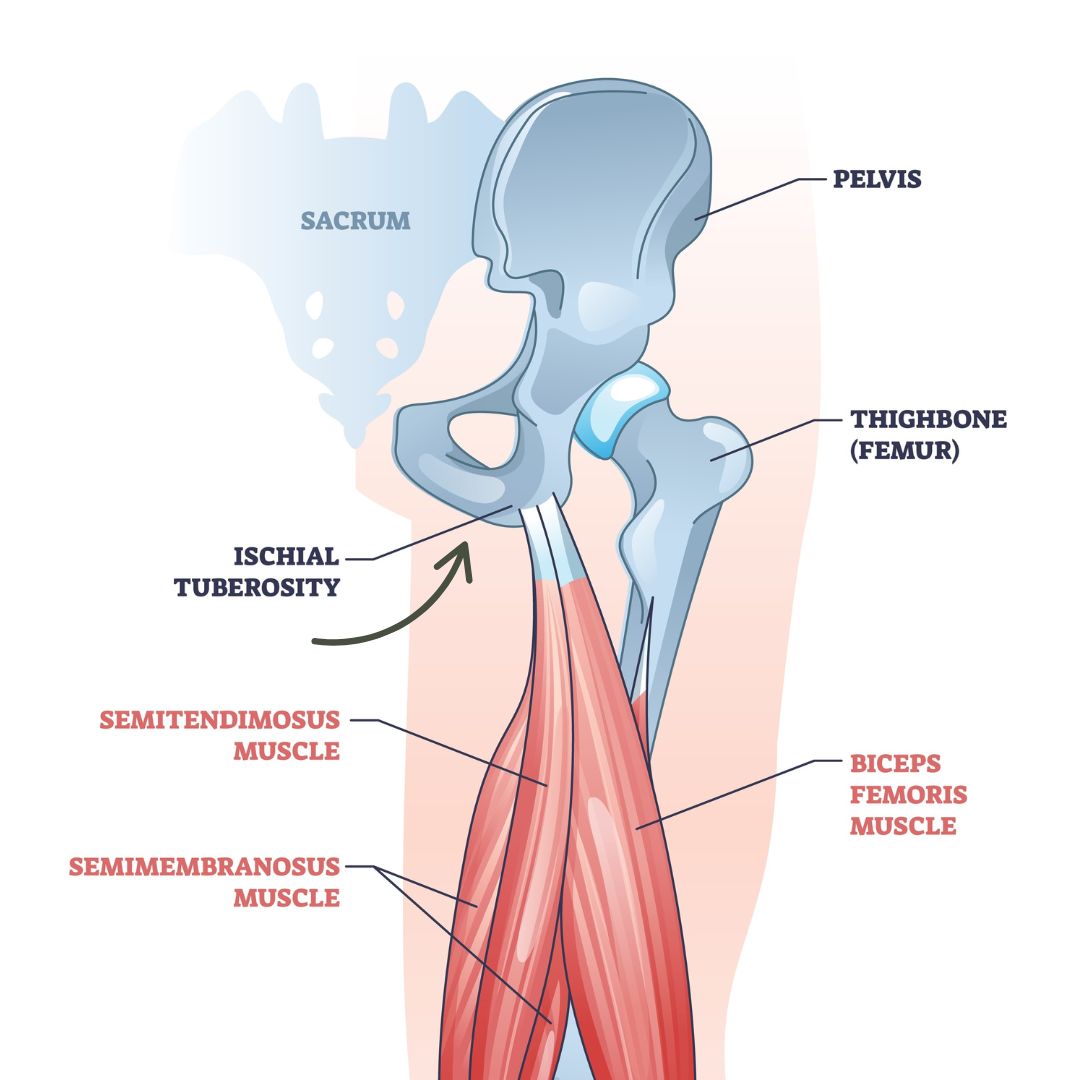
Ischial Bursitis (Sits Bone Pain)
What is it?
Inflammation of the bursa (fluid filed sac) under your sits bone, often caused by prolonged sitting, tight hamstrings, or overuse. It usually feels like a deep ache or sharp pain in the butt, especially when sitting, stretching, or going uphill.
-
Prolonged sitting on hard surfaces: Especially common in cyclists, drivers, or desk workers.
-
Hamstring overuse or tightness: The hamstring attaches at the ischial tuberosity (sits bone), and chronic tension can irritate the bursa underneath.
-
Poor glute activation: If the glutes aren’t pulling their weight, the hamstrings often compensate, leading to overload at their attachment point.
-
Pelvic floor dysfunction and overactive adductors (inner thigh): Tight pelvic floor muscles and adductors can increase tension in the back side of the pelvis and contribute to ischial compression. The adductors connect near the area as well.
-
Fascial restrictions or poor lymphatic drainage: These can lead to chronic inflammation or tissue irritation in the area.
-
Posture and spinal alignment changes: Especially lumbar extension or anterior pelvic tilt, which compresses the bursa.
-
Repetitive impact or trauma: Like falls on the buttocks or long-distance running without proper recovery.
- Hormonal shifts (ie menopause) During menopause, lower estrogen levels can lead to decreased tissue elasticity and increased tension around the pelvis, making ischial bursitis more likely.
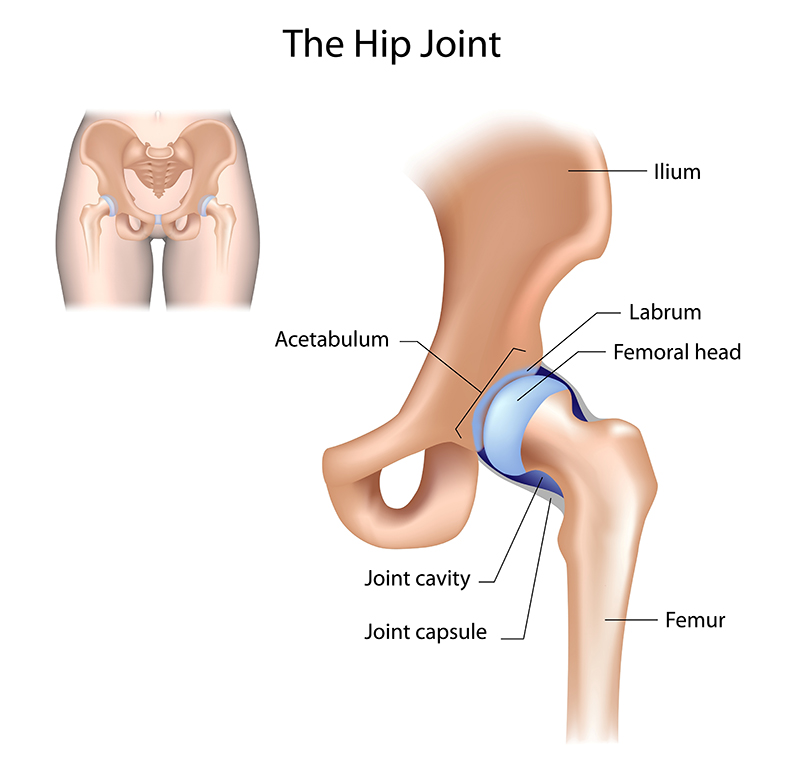
Hip Labral Tear
Hip Labral Tear
What Is It?
The labrum is a suction cup like cartilage that helps to stabilize the “ball and socket” joint of the hip. This means that a person may feel catching, clicking or grinding in the joint due to the femoral head coming in contact with the tear.
When this is torn, it can cause pain or feeling of instability during daily activities or even high level activities such as running.
-
Hip impingement (FAI): Irritation/pinching along the hip joint
-
Joint instability or hypermobility: The head of the femur has extra mobility, putting extra strain on the labrum.
-
Repetitive motion or overuse: Especially in dancers, runners, or athletes doing deep squats or twisting.
-
Trauma or injury: Like a fall, car accident, or sudden pivot.
-
Poor core and glute stability: This forces the hip flexor and labrum to overwork.
-
Referred pain from the spine (T12-L1): Nerve irritation here can mimic hip or even pelvic symptoms (such as vaginal pain)
-
Underlying fascial or lymphatic restrictions: These can cause chronic tension in the front of the hip and pelvis, increasing strain.
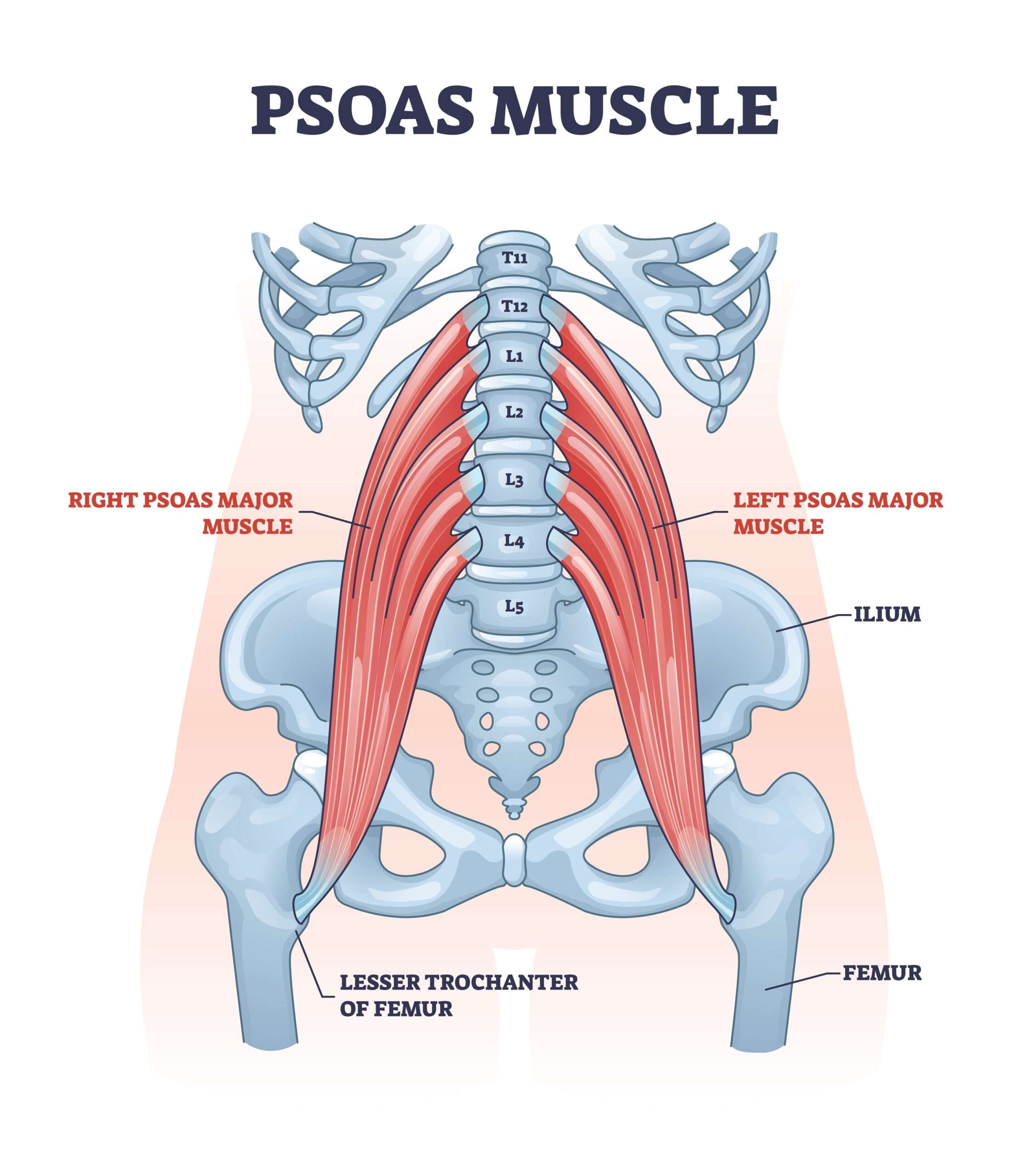
Hip Flexor
Hip Flexor Pain
What Is It?
Hip flexor pain is discomfort in the front of the hip or groin area, often caused by overuse, prolonged sitting, or compensation from other areas like the low back.
Common causes include:
-
Hip Impingement (FAI): This can cause the hip flexor to activate as a stabilizer, leading to overuse and irritation.
-
Constipation: The colon sits right in front of your hip flexors. If you haven’t pooped, or haven’t pooped as much, it can create pressure and pain in the area.
-
Lymphatic Congestion: Impaired drainage in the abdomen can lead to swelling and tension through the tissues, putting extra load on the hip flexor. Often people are unaware of this.
-
Restricted Fascial Mobility: If the fascia around your abdomen is restricted your hip flexor can’t glide as freely which means more strain on the hip flexor
-
Referred Pain from the Lumbar Spine: Nerve irritation or dysfunction in your low back can mimic or contribute to hip flexor pain
-
Limited Thoracic (Mid Back) Mobility: If your upper back isn’t moving well, your lower body has to compensate so the hip flexors will kick in to help (especially with walking)
-
Impaired Core Strength: Without proper support from your deep core (not just the six-pack), your hip flexors may overwork just to keep you upright.
- Endometriosis: This can be due to nerve irritation, fascial restrictions, or organ adhesions that limit pelvic and hip mobility, leading to chronic tension and compensation.
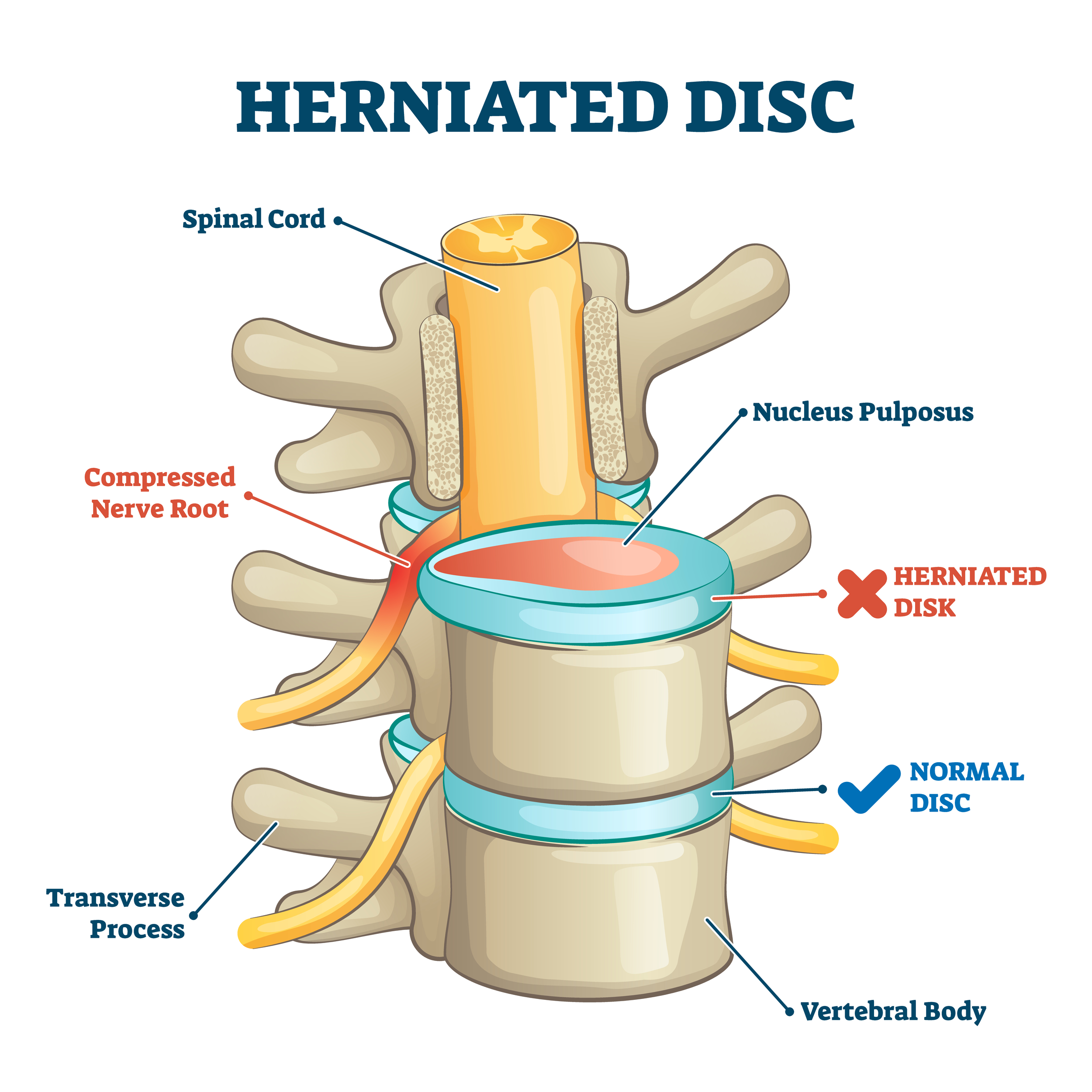
Disc Herniation
Lumbar Disc Herniation
What Is It?
A lumbar disc herniation happens when the inner gel-like center of a spinal disc pushes out through a tear in the outer layer, and can sometimes press on nearby nerves.
-
-
Rounded shoulders and mid-back stiffness: Limits thoracic mobility, forcing the low back to overcompensate.
-
Poor hip mobility: When the hips don’t move well, the lumbar spine takes on the load.
-
Tight pelvic floor muscles: Can restrict pelvic and spinal movement, contributing to compensation patterns.
- Impaired diaphragm function or shallow breathing: Reduces intra-abdominal pressure and core stability, leaving the lumbar spine unsupported.
-
Impaired deep abdominal and spinal activation: With impaired muscular support, the lumbar spine can be more vulnerable.
-
Gait dysfunction: Altered walking patterns can lead to chronic loading and wear on the discs.
-
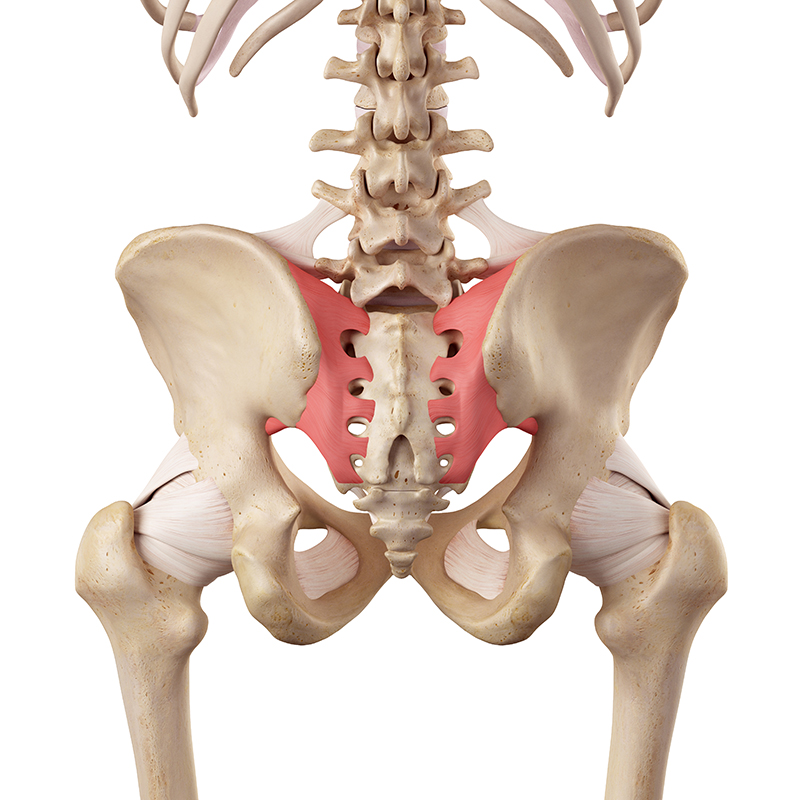
SI Joint Pain
SI Joint Pain
What Is It?
The SI joint connects your spine to your pelvis and acts as a stable shock absorber, designed for minimal movement. True SI joint dysfunction is less common and usually shows up in cases of hypermobility, postpartum ligament laxity, or trauma. Otherwise, pain in this area is often referred from the lumbar spine, hip, or pelvic floor.
-
Referred pain from nearby areas: The lumbar spine, pelvic floor, or hip can all refer pain to the SI joint, which leads to diagnosis based on location, not the true source.
-
Pregnancy and postpartum changes: Hormonal shifts cause ligament laxity, which reduces SI joint stability.
-
Hypermobility: When ligaments are naturally more lax (as in EDS, ehlers danlos, or joint hypermobility), the SI joint has to rely more on muscular support, which often fatigues.
-
Repetitive single-leg activities: Running, hiking, or asymmetrical training can create micro-instability over time.
-
Trauma: Falls, car accidents, or hard landings can overload the SI joint and surrounding tissues.
-
Pelvic floor dysfunction: Tight or imbalanced pelvic floor muscles can pull unevenly on the pelvis, impacting SI joint mechanics.

